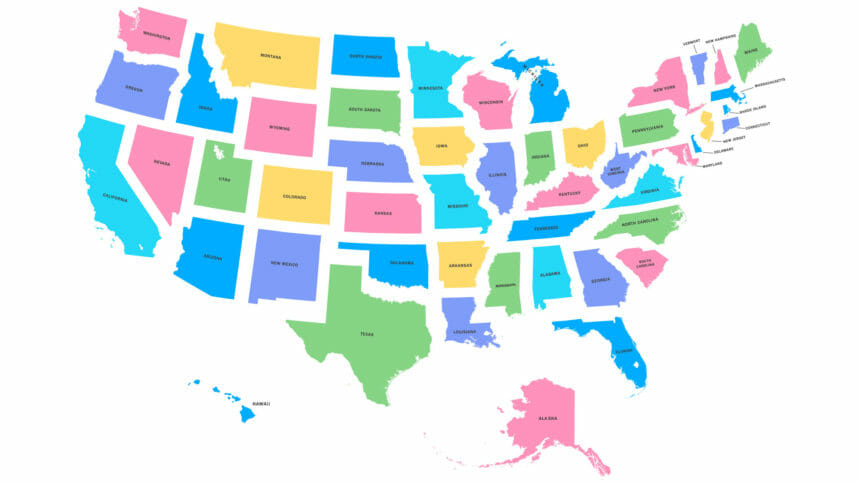
The federal government’s overlooking of assisted living communities in COVID-19 prevention and containment efforts has led to a patchwork of guidelines among states, resulting in uneven effects across the country, according to a new Kaiser Family Foundation report.
“[G]iven the paucity of state-reported data on case and death numbers in assisted living facilities specifically, the picture of disease incidence and mortality in these facilities is profoundly incomplete and undoubtedly an undercount,” said the authors of “Under the Radar: States Vary in Regulating and Reporting COVID-19 in Assisted Living Facilities.”
The report examines how states are regulating assisted living communities in response to the COVID-19 pandemic based on three key measures identified by the Centers for Medicare & Medicaid Services for nursing homes: visitor limitations, daily staff screening and universal use of personal protective equipment.
As of June 4, more than 43,000 COVID-19-related resident and staff deaths were reported in long-term care facilities (not strictly assisted living) — a conservative estimate because not all states publish data, according to the authors. Among 41 states reporting data, long-term care residents account for 50% or more of COVID-19 deaths in 27 states, creating a sense of urgency among policymakers, the industry, residents and their families, the authors said.
The report found:
- 10 states impose restrictions on assisted living communities that are identical to those established by CMS for nursing facilities, including prohibiting visitors and requiring staff screening and use of PPE.
- A majority of states (26 plus Washington, D.C.) prohibit visits to assisted living communities, but only 27 states recommend (rather than require) daily staff screening and use of PPE.
- Only 16 states report COVID-19 cases and / or death data for assisted living communities. Only six states report COVID-19 deaths in assisted living communities specifically.
- Among 11 states reporting COVID-19 cases for assisted living communities, a total of 9,513 cases among residents and staff were reported. Among the six states reporting deaths, a total of 1,215 deaths were reported.
In a majority of states, regulatory measures to protect assisted living residents and staff from the virus are less stringent than federal recommendations for nursing faculties, according to the report. Without uniform surveillance and reporting, the authors note, the extent to which the communities are adhering to state guidelines — or whether states are monitoring enforcement — is unknown.
Testing is another area of wide variation, according to the report. Some states instituted universal testing of nursing facility residents and staff, whereas others states, such as Connecticut and New York, now mandate universal testing of staff in both nursing homes and assisted living communities.
The situation “mirrors a larger national trend in the COVID-19 response,” the authors said.
“Some states have taken more aggressive actions than others, and the federal government assumes a backup role,” the report states. “This state-by-state approach to the COVID-19 pandemic may result in uneven rates of illness, hospitalizations and mortality among assisted living residents and staff across the country.”