The Health Resources and Services Administration is set to send $413 million in Provider Relief Fund Phase 4 general distribution payments to more than 3,600 providers across the country this week.
General distribution payments from the fund, totaling almost $12 billion, have been sent to more than 82,000 providers in all 50 states, Washington, D.C., and five territories since November 2021. Those payments are in addition to HRSA’s distribution of almost $7.5 billion in American Rescue Plan payments sent to more than 44,000 rural providers across the country over the past four months.
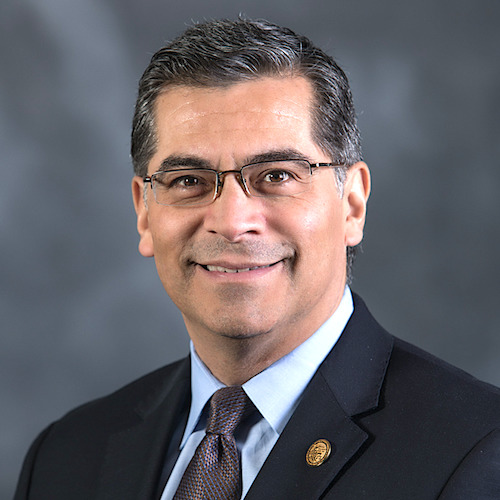
“These funds have helped save lives throughout the pandemic,” Health and Human Services Secretary Xavier Becerra said in a Tuesday press release. “As we continue to make progress in defeating COVID-19, it’s important to keep supporting our providers with the resources they need so we can all build back better and healthier than before.”
PRF general distribution payments received in the first half of 2022 can be used until June 30, 2023. Including the latest payments, approximately 89% of all Phase 4 applications have been processed. Remaining applications require additional manual review, and HRSA said it is working to process them as quickly as possible.
Failure to report
Providers began receiving failure to report notifications March 14 for one of three possible reasons, according to the American Health Care Association / National Center for Assisted Living:
- A SNF targeted allocation was filed at the parent level rather than at the subsidiary level.
- Sections were omitted.
- Data entry errors were made.
“The 30-day repayment notification language in these transmittals is confusing,” AHCA / NCAL said. “No funds should be returned to HRSA unless a provider receives a Demand Letter. Before Demand Letters, providers will be offered the opportunity to correct reporting errors or for HRSA to determine whether the notification was sent in error.”


